Fact Checked
Intus Healthcare’s writers, customer service team, and sleep experts review and ensure this information is accurate.
Last updated on April 8th, 2024 at 01:25 pm
Obstructive Sleep Apnoea (OSA) is a sleep disorder that causes pauses in breathing throughout sleep. The breathing disruptions are caused by periodic narrowing or blockages of the upper airway. The condition is more common in men, and it’s prevalence in women is often less noticeable. This article will explore how OSA affects women, its potential causes, and the importance of treating the condition for overall health.
Table of Contents
Sleep Apnoea symptoms in women
Research suggests that 425 million adults aged 30–69 worldwide could have moderate to severe Sleep Apnoea (1), making it one of the most common sleep disorders. The condition affects males and females differently due to differences in fat distribution, collapsibility and length of the upper airway, arousal response, and hormones. As the condition often goes unnoticed in women, it can seriously impact women’s health. Diagnosing Sleep Apnoea in women can be more difficult as the symptoms and causes can be slightly different.
To help you identify the condition, look out for these signs of Sleep Apnoea in women:
- Morning headaches
- Insomnia
- Daytime fatigue
- Mood swings
- Loud snoring
- Hallucinations
- Restless legs
- Anxiety and depression
- Memory loss
- Teeth grinding
- Choking in sleep
- Frequent urination during the night
Research has found that snoring is one of the most significant signs of OSA in both genders (2). However, many women often try to hide that they snore. By concealing their snoring, it can make it harder to identify if the condition is present and delay treatment. A study also found that middle-aged women with low serum oestrogen and progesterone levels are more likely to snore and report signs of OSA than younger women(3).
What increases the risk of Sleep Apnoea in women?
Many women may be at a higher risk of developing Sleep Apnoea due to differences in anatomical features, lifestyle choices and genetics. Specific factors that can increase this risk include:
Metabolic syndrome: Obesity is often an element of metabolic syndrome, which includes conditions such as insulin resistance and hypertension. Metabolic syndrome and its associated inflammation can contribute to structural changes in the upper airway and increase the risk of OSA. Women with metabolic syndrome or related conditions may be prone to developing OSA, especially if they have excess fat deposition in the upper body.
Genetics: Certain genetic and anatomical factors may increase women’s risk of OSA. For instance, women with a family history of OSA or anatomical abnormalities such as a narrow airway, deviated septum, or enlarged tonsils may be at higher risk. Fat distribution patterns can also interact with these factors, further increasing the likelihood of airway obstruction during sleep.
Age: Hormone changes in women contribute to OSA, which is why women tend to develop the disorder later in life often during or after menopause.
Hormone levels: As mentioned earlier in this article, hormonal imbalances can increase the risk of Sleep Apnoea.
Lifestyle habits: Drinking alcohol, smoking, and insufficient exercise can all contribute to an increased risk of the condition.
If you have symptoms or risk factors of OSA, it is essential to understand if the condition is present.

Sleep Apnoea Test
A quick and easy way to confirm if you do or do not have Sleep Apnoea is by taking a sleep test.
The Sleep Apnoea test requires one night of sleep data, and the results are sent to you within two working days. Taking the test puts you closer to understanding if you have overlap syndrome.
Upper airway differences in men and women
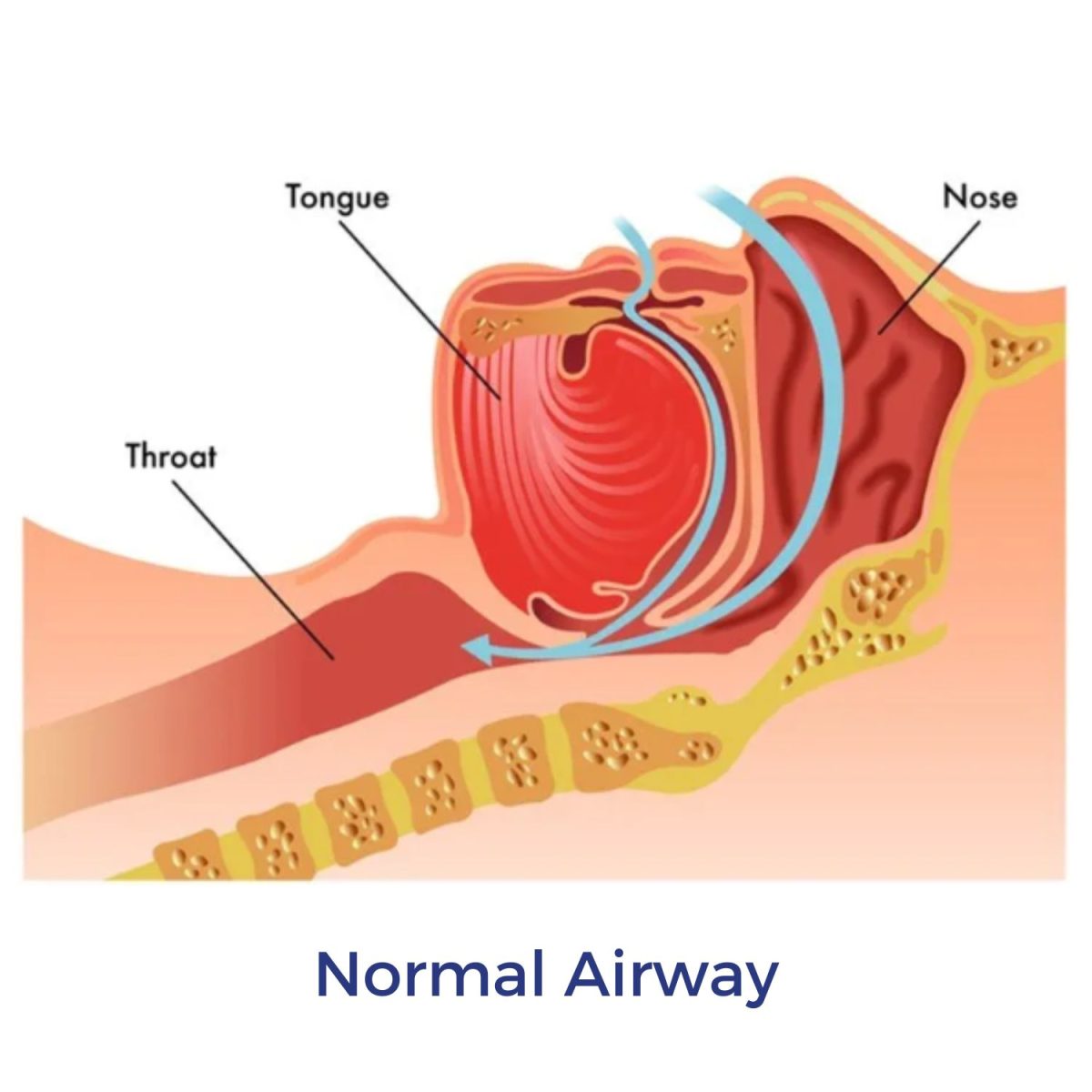
Obstructive Sleep Apnoea is primarily caused by the upper airway collapsing during sleep, making breathing harder. Medical imagery has shown that the upper airway anatomy including airway length, the soft palate, the tongue, and the amount of soft tissue in the throat are all generally smaller in women than in men (4).
These structural differences contribute to reduced upper airway collapse in women. Men commonly have longer, softer tonsils, more elongated soft palates and a larger tongue, which increases the vulnerability of the airway to collapse during sleep.

Weight distribution in men and women
Obesity and a higher BMI (Body Mass Index) increase the risk of developing OSA in both genders. Fat accumulation in the upper body, around the neck and throat, can increase pressure on the airway during sleep, increasing the likelihood of collapse and causing breathing difficulties.
Women may weigh more than men with the same AHI (Apnoea Hypopnoea Index), as women are predisposed to store more body fat than men. Women with central obesity (fat accumulation around the waist and neck) are at a higher risk of OSA compared to those with peripheral obesity (fat accumulation around the hips and thighs). As central obesity increases the risk of an airway obstruction.
Sleep Apnoea and female hormones
Hormone levels can impact the risk of sleep disturbances, including Sleep Apnoea. The relationship between OSA and your hormones is complex, and the two can have a cyclical effect on each other. The body’s sex hormones, such as progesterone, androgens, oestrogen, and testosterone, directly affect breathing during sleep. Sleep deprivation due to OSA can also impact hormone levels and trigger a rise in adrenaline levels.
Women may be more likely to experience symptoms of OSA due to hormones during pregnancy, menopause, or certain times of the menstrual cycle. This is caused by fluctuations in hormones such as oestrogen, testosterone and progesterone.
Pregnancy and Sleep Apnoea
The risk of developing Sleep Apnoea increases during pregnancy due to significant hormonal changes. These hormonal changes can lead to increased mucus production in the nose, making congestion more likely and increasing the risk of snoring and Sleep Apnoea. Additionally, the higher levels of progesterone may contribute to relaxation and narrowing of the airway, further increasing the risk of OSA during pregnancy. Weight increases during pregnancy can add pressure to the airway, making breathing more difficult.
Pregnant women are also more likely to sleep on their backs, and this sleeping position increases the risk of airway blockage. However, for many women who develop the condition during pregnancy, its severity may reduce after giving birth.
How does OSA affect pregnancy?
The sleep condition can increase the risk of:
- Prolonged labour
- Unplanned caesarean sections
- Preeclampsia
- Gestational diabetes
The breathing disruptions caused by OSA can increase blood pressure, which can reduce blood flow to the baby, affecting the baby’s oxygen levels and nutrient supply.
Continuous sleep interruptions during pregnancy can reduce the release of growth hormones that are normally released during sleep. This can potentially impact the baby’s growth and development leading to various health complications for the baby. Research suggests that up to 27% of pregnant people may develop OSA (5).
PCOS and Sleep Apnoea
Polycystic Ovary Syndrome (PCOS) is a female health condition that affects hormonal levels that can influence fertility and other aspects of life.
PCOS encompasses a group of symptoms, including absence or irregular menstruation, difficulty getting pregnant, fatigue, weight gain, acne, hair thinning and abnormal hair growth. PCOS is a common condition affecting every 1 in 10 women in the UK (6), and often, the way the condition affects each woman varies.
Those with PCOS often experience increased levels of androgens; these are male hormones that women also have. An increase in androgens can raise the risk of Sleep Apnoea by influencing fat distribution around the airway and affecting upper airway anatomy and muscle tone.
Androgens also influence metabolism and can contribute to insulin resistance and metabolic syndrome (a cluster of conditions including high blood pressure and elevated blood sugar). Insulin resistance is when cells become less responsive to the effects of insulin, leading to elevated blood sugar levels. These metabolic disturbances are often associated with obesity and can further exacerbate the risk of developing OSA and type 2 diabetes.
As well as higher androgen levels, those with PCOS commonly experience menstrual irregularities and fluctuations in oestrogen and progesterone. These hormonal changes, particularly during the menstrual cycle, can affect upper airway muscle tone and respiratory control during sleep.
Women with PCOS often have chronic low-grade inflammation and increased oxidative stress. These factors can lead to structural changes in the upper airway tissues, making them more prone to collapse during sleep, leading to OSA.
A study found that the risk of OSA is at least 5-to-10-fold higher in women with PCOS compared to those without PCOS (7).

Sleep Apnoea & Menopause
As women age, the likelihood of developing Sleep Apnoea increases through weight and hormonal changes. The average age for menopause is between 45 and 55 for most women.
Menopause is when the ovaries no longer produce oestrogen and progesterone, which can affect many systems and processes in the body, including sleep.
Before menopause, women typically have higher levels of oestrogen and progesterone; these hormones maintain the airway’s muscle tone and help to prevent them from collapsing. However, these hormones decline during perimenopause (the transition to menopause), increasing the risk of airway collapse, a key characteristic of Sleep Apnoea.
Many women experience weight gain during menopause, particularly around the abdomen and neck, due to lower oestrogen. The excess weight can further increase the risk of OSA.
Menopausal women often experience poor sleep quality and sleep fragmentation, which can increase the severity or worsen existing effects of the sleep condition.
Menopause is associated with changes in metabolism, including decreased energy expenditure and alterations in fat distribution. These metabolic changes can affect how the body converts food into energy and contribute to weight gain and insulin resistance.
Many symptoms of OSA overlap with the symptoms of menopause, including:
- Mood changes
- Trouble sleeping
- Weight gain
- Urinary problems
- Poor concentrations
- Irregular periods
- Hot flushes
If you are experiencing perimenopause or menopause and are concerned that some of your symptoms may be due to OSA, you should speak with your healthcare provider for guidance. Menopause and sleep disorders often go hand in hand but can be managed with correct treatment and lifestyle adjustments.
Treatment
There are different severities of OSA, ranging from mild to severe. Recommended treatment can vary depending on the severity and a person’s individual case. Treatment includes:
CPAP therapy: Continuous Positive Airway Pressure (CPAP) is the most widely used treatment method. The therapy involves using a CPAP machine, mask and tubing to deliver a continuous stream of pressurised air to the user’s airway during sleep. The pressurised air keeps the airway open during sleep to prevent pauses in breathing.
MADs: Mandibular Advancement Devices (MADs) are mouth guards designed for Sleep Apnoea and snoring. It works by gently pulling the lower jaw forward to prevent airway collapse. This method of treatment is most appropriate for those with mild OSA.
Positional therapy: This treatment is suitable for positional OSA and works to encourage the patient to sleep on their side. Sleeping on your side helps keep the airway open, preventing the tongue from falling back and creating a blockage.
The Somnibel Positional Sleep Therapy Trainer is a popular positional therapy treatment. The Somnibel is a small device that sits on the forehead, creating light vibrations when the user turns onto their back during sleep. The vibrations encourage the user to roll back onto their side.
Lifestyle changes: Patients are often advised to make lifestyle adjustments alongside treatment. These changes may include exercising more regularly, consuming less alcohol and quitting smoking.
Treatment is essential in those with OSA as when it is left unmanaged, it can cause the development of further health conditions.
The underdiagnoses of OSA in women
The prevalence of Obstructive Sleep Apnoea in women often goes unnoticed and should be addressed. If you have any signs of the condition, you should discuss this with your healthcare provider.
At Intus Healthcare, we specialise in OSA treatment and testing and can provide all you need to restore quality sleep.
Related article: Do women need more sleep than men?
REFERENCES
- Benjafield, A. V., Ayas, N. T., Eastwood, P. R., Heinzer, R., M Ip, M. S., Morrell, M. J., Nunez, C. M., Patel, S. R., Penzel, T., Pépin, L. D., Peppard, P. E., Sinha, S., Tufik, S., Valentine, K., & Malhotra, A. (2019). Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. The Lancet. Respiratory Medicine, 7(8), 687. Available at: https://doi.org/10.1016/S2213-2600(19)30198-5. Accessed: 26.02.2024
- Young T, Hutton R, Finn L, Badr S, Palta M. (1996) The gender bias in sleep apnea diagnosis. Are women missed because they have different symptoms? Arch Intern Med. PMID: 8944737. Available at: https://pubmed.ncbi.nlm.nih.gov/8944737/. Accessed: 26.02.2024
- Sigurðardóttir, E. S., Gislason, T., Benediktsdottir, B., Hustad, S., Dadvand, P., Demoly, P., Franklin, K. A., Heinrich, J., Holm, M., Jõgi, R., Leynaert, B., Lindberg, E., Martinez-Moratalla, J., De Aja, L. S., Pesce, G., Pin, I., Raherison, C., Pereira-Vega, A., Real, F. G., . . . Triebner, K. (2022). Female sex hormones and symptoms of obstructive sleep apnea in European women of a population-based cohort. PLOS ONE, 17(6), e0269569. Available at: https://doi.org/10.1371/journal.pone.0269569. Accessed: 26.02.2024
- Thurnheer R, Wraith PK, Douglas NJ. Influence of age and gender on upper airway resistance in NREM and REM sleep. J Appl Physiol (1985). 2001 Mar;90(3):981-8. doi: 10.1152/jappl.2001.90.3.981. PMID: 11181609. Available at: https://pubmed.ncbi.nlm.nih.gov/11181609/. Accessed: 26.02.2024
- Louis, J., & Piem, G. W. (2023). Obstructive sleep apnea in pregnancy. In V. Berghalla, & N. Collop (Eds.). Available at: https://www.uptodate.com/contents/obstructive-sleep-apnea-in-pregnancy. Accessed: 26.02.2024
- Polycystic ovary syndrome (2022) NHS UK. Available at: https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/. Accessed: 26.02.2024
- Ehrmann, D. A. (2012). Metabolic dysfunction in PCOS: Relationship to obstructive sleep apnea. Steroids, 77(4), 290-294. Available at: https://doi.org/10.1016/j.steroids.2011.12.001. Accessed: 26.02.2024.








